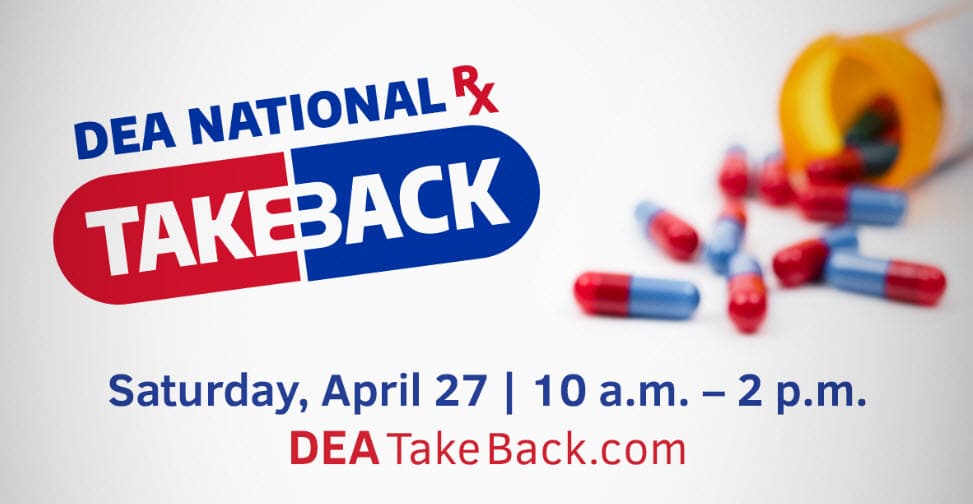
On Saturday, April 27, from 10 a.m. to 2 p.m., The Council on Recovery and the U.S. Drug Enforcement Administration will give the public its 17th opportunity in nine years to prevent pill abuse and theft by ridding their homes of potentially dangerous expired, unused, and unwanted prescription drugs.
Bring your pills for disposal to The Council at 303 Jackson Hill Street in Houston. (We cannot accept liquids or needles or sharps, only pills or patches). This drive up/drop-off service is free and anonymous, no questions asked. The Council’s drive-through covered portico will keep everyone dry in the event of rain. Additional security personnel will also assure the safety of everyone who participates in the event.
Last fall Americans turned in nearly 460 tons (more than 900,000 pounds) of prescription drugs at more than 5,800 sites operated by the DEA and almost 4,800 of its state and local law enforcement partners. Overall, in its 16 previous Take Back events, DEA and its partners have taken in almost 11 million pounds—nearly 5,500 tons—of pills.
This Take Back initiative addresses a vital public safety and public health issue. Medicines that languish in home cabinets are highly susceptible to diversion, misuse, and abuse. Rates of prescription drug abuse in the U.S. are alarmingly high, as are the number of accidental poisonings and overdoses due to these drugs. The Substance Abuse and Mental Health Services Administration’s National Survey on Drug Use and Health shows year after year that the majority of misused and abused prescription drugs are obtained from family and friends. These include someone else’s medication being stolen from the home medicine cabinet.
In addition, Americans are now advised that their usual methods for disposing of unused medicines—flushing them down the toilet or throwing them in the trash—both pose potential safety and health hazards.
For more information about the disposal of prescription drugs or about the April 27 Take Back Day event, go to www.DEATakeBack.com or call The Council at 713-942-4100 or contact us online.
