The following article was recently published on the research page of the Recovery Research Institute website. It explores a new study that indicates Latinos have the lowest treatment seeking rates compared to people of other racial and ethnic backgrounds.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
National studies have shown that individuals who identify as Latino are less likely to seek treatment for substance use disorder or complete treatment at specialty treatment facilities. Barriers to treatment engagement by race and ethnicity have been examined in only a few national studies and results are inconclusive. Identifying barriers to treatment is a foundational step that will allow for public health planning aimed at addressing barriers. The purpose of this in–depth qualitative study was to gain a better understanding of barriers to specialty treatment for substance use disorder that are more prominent among Latinos than other racial and ethnic groups.
HOW WAS THIS STUDY CONDUCTED?
From 2017-2018 the authors conducted a qualitative study which consisted of telephone interviews with participants from Riverside, Los Angeles, San Diego, and Oakland, CA; Brooklyn, NY; Chicago, IL; Miami, FL; and San Antonio, TX, recruited via craigslist (i.e., a web-based advertising platform) to compare barriers to treatment utilization among racial and ethnic groups.
WHAT DID THIS STUDY FIND?
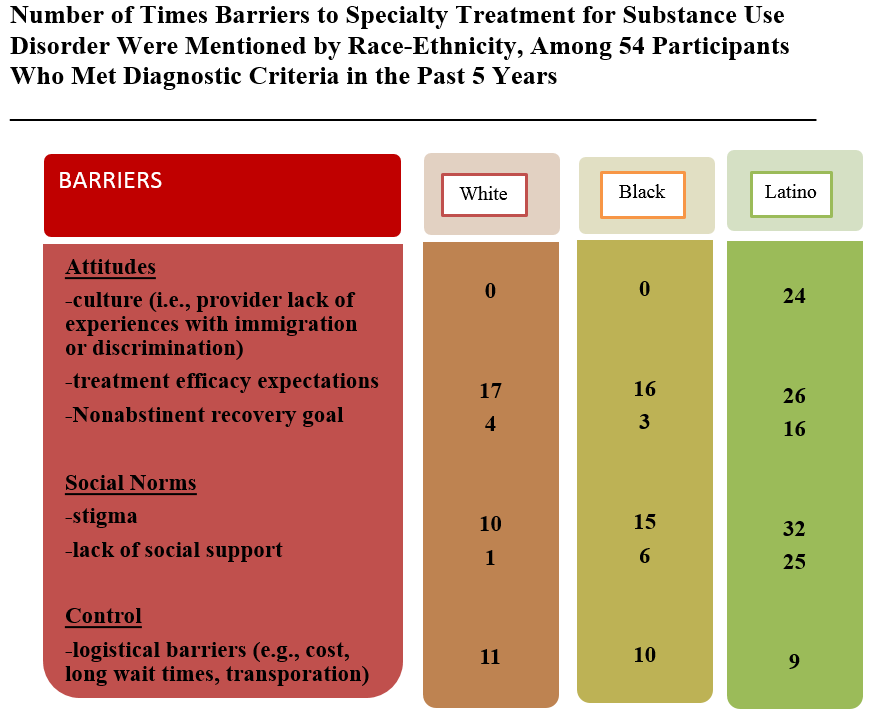
Figure 1. Source: Pinedo et al, 2018
Latinos reported attitudinal barriers to specialty treatment more than other racial and ethnic groups (i.e., cultural, perceived treatment efficacy, and non-abstinent recovery goals). Overall, Latinos commonly felt specialty treatment providers did not understand their unique needs and experience. Specifically, they perceived healthcare providers to be unfamiliar with cultural issues such as discrimination and immigration. Providers were, therefore, discussed in terms of not being able to relate to personal experiences associated with being Latino including alcohol or other drug use which was in turn associated with low treatment efficacy. Being able to have a recovery goal of moderated alcohol use, and not complete abstinence, emerged as a larger barrier for Latinos in seeking treatment at specialty facilities. Its is unclear if these barriers could vary according to generation, meaning, foreign versus native born Latinos.
Social norms barriers towards specialty treatment (i.e., stigma and lack of social support) were more pronounced among Latinos than their White and Black counterparts. Stigma for seeking treatment was strong across all groups but most frequently mentioned by Latinos. Lack of social support from family emerged because it was viewed as “confirming” they had a problem and may tarnish the family.
Control over specialty treatment specifically logistical barriers, such as lack of health insurance, cost of treatment, transportation, and long wait times were highlighted by all racial and ethnic groups during interviews, however, showed no considerable differences in number of times mentioned between groups.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study identified specific barriers that discourage individuals who identify as Latino with alcohol or other drug use disorders from seeking treatment, and compared these to other racial and ethnic groups. Barrier identification is important because Latinos seek treatment at about half the rate as their White counterparts although higher estimates have been reported. Latino expectations that providers do not understand cultural issues like discrimination and immigration was an attitude barrier for seeking treatment. Researchers have suggested acknowledging important social contexts such as immigration and discrimination experiences in the delivery of specialty treatment for substance use disorders may increase service use. Latinos low expectations around treatment efficacy where rooted providers having no lived experience with alcohol or other drug problems and therefore are unable able to relate. Treatment facilities may need to promote their use of, or integration with, peer services as a means of showing that lived experience can be a part of the treatment process. Clinicians should be prepared to work with patients whose recovery goals include an initial goal of moderate alcohol use given about half of people in the US who have resolved a problem with alcohol or other drugs are not completely abstinent.
Stigma was heavily endorsed by Latinos including concerns over being seen by colleagues at a specialty treatment facility. To address this barrier, treatment centers might offer telemedicine which is when treatment is delivered using telecommunications technology like Skype but specially designed for secure health care communication. In fact, a National Recovery Study found that individuals who identify as Hispanic were over one a half times as likely than White individuals to use recovery-related online technology. So, this may be a way to engage more Latinos with substance use disorder in treatment.
LIMITATIONS
- Qualitative studies like this use smaller samples to obtain richer ideas and explanations. This study was on only on a total of 54 individuals, of whom only 20 were Latino, recruited by advertisement, so it’s unclear to what extent findings may generalize to Latinos with substance use disorder as a whole. Particularly given the participants were assessed in terms of meeting diagnostic criteria over a 5 year window instead of 12 months, which is more standard.
- The barriers to treatment seeking identified in this qualitative study should be further tested in larger samples, and ideally, in a national study to determine the US prevalence of these barriers among racial and ethnic groups.
- Latino alone is a large group and there may be generational issues to consider in these outcomes related to foreign versus native born Latinos.
BOTTOM LINE
- For individuals & families seeking recovery: This study of barriers to treatment for substance use disorder found that expectations of low efficacy were common. This low perceived efficacy of treatment was related to experiences with treatment providers who had no lived experience with substance use disorder, or providers who were perceived to not understand stressful cultural issues like immigration and discrimination and its association with the onset, clinical course, and remission of substance use disorder. Talk to a treatment provider about setting expectations around the likelihood of remission, their use or integration with peer services, and provider cultural competency.
- For scientists: This qualitative study found that social norms around low family support and acceptability of seeking treatment may be a barrier among individuals who identify as Latino. Preventative interventions aimed at adolescents and emerging adults that seek to improve the acceptability of using professional services for substance use disorders may have lasting impacts on creating a future culture of support and reduced stigma, that extends to families and communities across generations. In addition, it is important to develop and test strategies that can help engage Latino individuals with services. For example, 12-step facilitation for Spanish speaking Latinos since they value lived experience.
- For policy makers: This was a qualitative study that examined barriers to specialty treatment for substance use disorder by race and ethnicity. Latino treatment seeking may be improved (and treatment seeking in general) by promoting the use of peer services (i.e., persons with lived experience in recovery), training providers in “cultural humility” in order to increase education around immigration and discrimination and its effect on recovery, and increasing privacy options during treatment. Telemedicine is an emerging option to increase privacy during treatment and provide access to hard to reach populations but research on effectiveness needs to be studied.
- For treatment professionals and treatment systems: This was a qualitative study that examined barriers to specialty treatment for substance use disorder among individuals who identify as White, Latino, and Black. Latino treatment seeking may be improved by (and treatment seeking in general) by accommodating non-abstinent recovery goals around alcohol use, promoting organizational integration with evidence-based peer services (i.e., persons with lived experience in recovery), training providers in cultural humility to increase education around immigration and discrimination and its effect on recovery, and increase privacy options during treatment seeking. Telemedicine is an emerging option to increase privacy during treatment and provide access to hard to reach populations but research on effectiveness needs to be studied. It may be important for clinicians to process and problem solve around Latinos’ mistrust in professional treatment and address the family and cultural barriers they may face if attending treatment (i.e., stigma or lack of social support).
CITATIONS
Pinedo, M., Zemore, S. & Rogers, S. (2018). Understanding barriers to specialty substance abuse treatment among Latinos. Journal of Substance Abuse Treatment, 94, 1-8.
