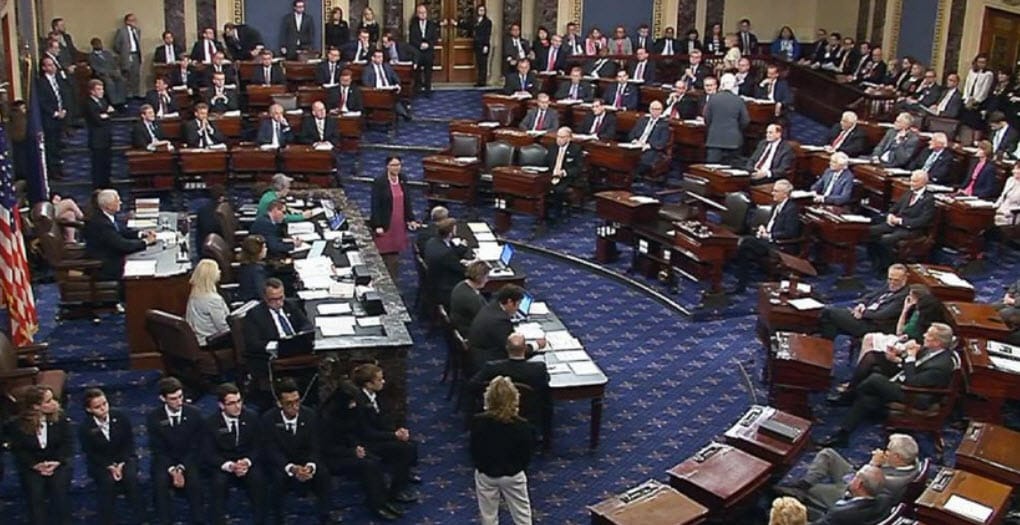
The Council on Recovery applauds the efforts of the United States Senate in passing the Opioid Crisis Response Act of 2018 by a vote of 99-1. The bill included the Substance Abuse Prevention Act, sponsored by Senators John Cornyn and Dianne Feinstein. The following press release was issued shortly after the bill passed:
U.S. Senators John Cornyn (R-TX) and Dianne Feinstein (D-CA) released the following statements after their Substance Abuse Prevention Act, a bipartisan bill to reauthorize drug abuse programs, passed as a part of The Opioid Crisis Response Act of 2018.
“Our nation continues to suffer from a drug crisis, and this critical legislation will combat the supply of opioids and help individuals and families suffering from substance abuse,” said Sen. Cornyn. “By including the Substance Abuse Prevention Act in this bill, we will be able to strengthen the ability of law enforcement and healthcare agencies to reduce addiction and support those in recovery.”
“Drug addiction and overdoses have reached crisis levels in our country,” Sen. Feinstein said. “In order to address this issue we must strengthen the agencies and programs that are focused on stopping drug use before it starts, dismantle drug trafficking organizations and expand access to treatment. This bill embraces that strategy by reauthorizing the Office of National Drug Control Policy and other successful initiatives like the Drug-Free Communities and High Intensity Drug Trafficking Areas programs. The bill also establishes new programs to provide law enforcement with tools, training and equipment to detect and prevent fentanyl-related overdoses and to ensure families and children have more access to substance abuse treatment.”
Background:
The Substance Abuse Prevention Act was originally introduced by Senators Cornyn and Feinstein to reauthorize drug abuse programs, and to provide assistance to various agencies so they can better combat opioid addiction and support those recovering from substance abuse.
- Office of National Drug Control Policy: Reauthorizes the Office of National Drug Control Policy (ONDCP) at the White House, which oversees Executive Branch efforts on narcotics control and ensures efforts complement and strengthen state and local anti-drug activates.
- Drug Abuse Prevention Programs: Reauthorizes several important programs under the ONDCP including the Drug-Free Communities Program and the High-Intensity Drug Trafficking Area Program and allows the ONDCP Director to participate in and expand opioid and heroin awareness campaigns which were authorized under the Comprehensive Addiction and Recovery Act (CARA).
- Drug Courts: Reauthorizes Department of Justice funding for drug courts, which provide targeted interventions for individuals with drug addiction and substance abuse disorders and allows non-profit organizations to provide important training and technical assistance to drug courts.
- Supporting Families with Substance Abuse Challenges: Provides resources to the Department of Health and Humans Services (HHS) for screening, treatment, supportive housing, and interventions in order to help support families as they battle substance abuse challenges.
- Better Substance Abuse Treatment: Directs the Government Accountability Office (GAO) to conduct a study on reimbursements for substance use disorder services and make recommendations in order to bring parity to and improve reimbursements.
- Educating Prescribers: Requires Attorney General and HHS Secretary to complete a plan for educating and training medical practitioners in best practices for prescribing controlled substances.
- Supporting Education and Awareness: Allows the Attorney General to make grants available to entities that focus on substance use disorders and specialize in family and patient services.
- Sobriety Treatment and Recovery Teams: Authorizes the Director of ONDCP in coordination with SAMHSA to provide grants to establish Sobriety Treatment and Recovery Teams (START) to determine the effectiveness of pairing social workers and mentors with families that are struggling with substance use disorder and child abuse or neglect.
The following groups supported the Substance Abuse Prevention Act: the Community Anti-Drug Coalitions of America (CADCA), the Addiction Policy Forum, the National Association for Children of Addiction (NACoA), the Moyer Foundation, the National Council for Behavioral Health, the National District Attorneys Association, the Fraternal Order of Police, the National HIDTA Directors Association, the Partnership for Drug-Free Kids, the National Criminal Justice Association, the National Association of Police Organizations, and the National Association of Drug Court Professionals.
